
Wellbeing of Women announces Professor Hilary Critchley as the new Research Advisory Committee Chair
Wellbeing of Women has announced its Chair and Deputy Chair of its Research Advisory Committee.
We’re delighted to announce the funding of 17 new research projects tackling health inequalities and spanning the whole life course – from menstruation to menopause, pre-natal to postnatal, and gynaecological cancers.

Now in our 60th year of saving and changing the lives of women, girls and babies, we’re proud to have invested more than £750,000 in pioneering research.
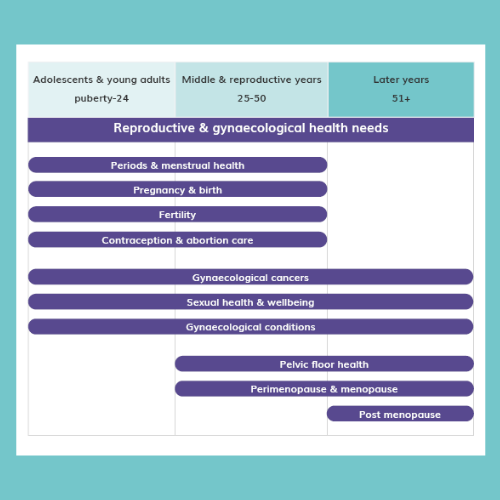
Wellbeing of Women is the only UK charity that covers all of women’s gynaecological and reproductive health. Our history has seen some big advancements in healthcare for women, both in the UK and globally, from establishing the role of ultrasound in pregnancy, proving the link between cervical cancer and pregnancy, showing the effectiveness and safety of the COVID-19 vaccine in pregnancy, and most recently funding a groundbreaking trial of the first ever non-surgical, non-hormonal treatment for endometriosis.
However, there’s still a long way to go to improve prevention, diagnosis, treatment and management across the life-course.
Coercive control (CC) is a pattern of behaviours in a relationship where one person tries to exert control over another and is a type of abuse that can be very difficult to identify. Coercive control can lead to long-term poor health for both the victim and any children involved. In the very worst cases, it can escalate to homicide. Dr Anna Sydor, Cardiff University, is gathering what is known about identification of coercive control and what interventions can be used to support victims and their children, with the hope of improving outcomes in future.
Funded in partnership with the Royal College of Midwives and Burdett Trust for Nursing
Heavy menstrual bleeding is estimated to affect 1 in 3 women and is a key symptom of fibroids, endometriosis and adenomyosis. Currently, a lack of effective treatment options means many women need a hysterectomy to stop the bleeding. Using innovative new technologies to explore the DNA, molecules, cells and tissues of samples from women with HMB, Dr Dania Badran hopes to shed light on what’s driving the various conditions – and unlock new options for treatment development.
Abnormal uterine bleeding (AUB) can refer to heavy, irregular, or prolonged periods and affects around four million women in the UK. It can have a devastating impact on quality of life, lead to further health complications, and is a huge financial burden for women, their families, the NHS, and society. Despite how common and debilitating AUB is, it’s still an underfunded and under-researched area. We’re supporting co-leads Dr Jacqueline Maybin, Dr Gemma Sharp and their team to set the top 10 research priorities for the future of AUB via a James Lind Priority Setting Partnership. This will bring together the voices of patients, carers, and clinicians to find the most important areas of research need that also have the biggest impact for the women affected.
Fetal growth restriction is a condition where an unborn baby is smaller than expected or stops growing during pregnancy. It affects around 1 in 12 pregnancies and can result in pregnancy complications, premature birth, or stillbirth. Dr Michael Wilkinson, based at the University of Manchester, will lead a project in the lab to find out if low-dose steroids could improve blood flow to the placenta. If successful it could be the first step towards a new way of treating this condition.
Funded in partnership with the British Maternal and Fetal Medicine Society
Poor sleep following birth can have a negative impact on physical and mental health and delay recovery. Ms Jacana Bresson, based at Lewisham & Greenwich NHS Trust, will use her extensive experience working as a midwife in the NHS to study the factors that influence how well new mums sleep on the ward, and use this to come up with ways to improve sleep quality.
Funded in partnership with the Royal College of Midwives and Burdett Trust for Nursing
Female fertility preservation refers to preserving the ability of an individual to have a biological child at a time of their choosing via methods like egg-freezing. It is an important but under-researched field. Via an NIHR James Lind Alliance Research Priority Setting Partnership, Dr Jemma Barash, based at University College London, will work to set priorities in this field for future studies. The end goal is to improve care for people seeking fertility preservation for medical or social reasons.
Hypertensive disorders, including pre-eclampsia and eclampsia, put mother and baby at increased risk of negative outcomes. Women from ethnic minority backgrounds are more likely to get one of these conditions in pregnancy and when they do, they have more serious complications. Dr Charlotte Williams, based at the University of Bristol, is hunting for factors that make women from ethnic backgrounds more vulnerable. The aim is to develop a checklist that can be used clinically to identify those at most risk – ensuring they get the help they need earlier.
Caesarean sections (CS) are performed to save the life of mother or baby or to avoid complications, but the procedure carries risks. Despite it being a common procedure, it is not known if these are performed for the right reasons to the right women. Dr Amie Wilson, University of Birmingham, is testing a tool called C-WHY in the NHS to determine if there are differences in why caesarean sections are performed. She’ll investigate whether factors like ethnicity influence decisions on CS, and how this impacts outcomes. If successful, the system could be rolled out to improve outcomes and help to reduce care inequalities.
Funded in partnership with the Royal College of Midwives and Burdett Trust for Nursing
Sickle cell disease (SCD) is common among people of African heritage and can cause significant health problems during pregnancy. Right now, the only treatment for these women during pregnancy is to have blood transfusions, which can be risky and aren’t easy to get everywhere in the world. Dr Evangelia Vlachodimitropoulou, based at King’s College London, is exploring a new type of treatment in the lab. If successful, it could pave the way for a new strategy to prevent pregnancy complications for mums with this disease.
Hypertensive diseases of pregnancy (HDP) affect 60,000 women in the UK each year, and describe complications related to blood pressure. Women who had HDP have double the risk of cardiovascular problems after pregnancy but we don’t know who’s at highest risk. Using a range of data sources, Dr Jennifer Jardine plans to hunt for patterns and join the dots between HDP in pregnancy, ethnicity and long-term health outcomes. She hopes to identify those at highest risk and develop potential interventions to prevent HDP in women from ethnic minority groups.
Funded in partnership with the British Maternal and Fetal Medicine Society
Every year in the UK, 6000 women need to have a caesarean section under general anaesthetic, and nearly 1400 require admission to intensive care units. This can mean a mum is separated from her baby for weeks. This ‘absence at birth’ can lead to post-natal depression and suicidal thoughts, but very little research has been done to find ways of supporting families who experience this. Mrs Michelle Anderson, King’s College London, is working to bridge this gap in knowledge with the aim of preventing mental health issues in women and their partners.
Women with serious mental health problems are at particular risk of reproductive health issues including sexually transmitted diseases, unwanted pregnancy, and pelvic pain. Dr Pollyanna Cohen, University College London, plans to equip mental health professionals with the training and support they need to recognise reproductive health issues and refer patients to the correct services. If successful, this could dramatically improve sexual and reproductive health outcomes for an extremely vulnerable group.
Funded in partnership with the Faculty of Sexual and Reproductive Health
Not much is known about what women from ethnic minority communities in the UK think about contraceptive options, or what side effects they experience. Miss Fatima Nabage, at the University of Sheffield, plans to work with women from these communities to understand their experiences and needs, using their insight to co-design information leaflets about contraceptive side effects. She hopes this will improve access to contraceptive services, supporting overall wellbeing.
Funded in partnership with the Faculty of Sexual and Reproductive Health
Vulvodynia is persistent, unexplained pain, which is often described as burning, stinging, or soreness, in the female genital area (vulva). It is estimated to affect 8-10% of women and can negatively impact their personal, intimate and social lives. Miss Athena Lountzi, at the University of Stirling, will work with women affected, healthcare professionals and support organisations to understand which aspects of the condition are most important to address through research.
Funded in partnership with the British Society for the Study of Vulval Disease
Vulval lichen sclerosus (LS) is a skin condition that can cause splitting, thinning and whitening of the vulva, it affects 3 in 10 women, and is most common in women over 50. Alongside having a detrimental impact on quality of life, the condition also increases risk of vulval cancer. Current information on LS just isn’t good enough, resources for patients are lacking in detail and women report conflicting information from their healthcare professionals – leading to unnecessary distress and anxiety. Co-leads Dr Sophie Rees and Dr Caroline Owen and their team are working to remedy this. Working in partnership with patients, they’ll develop a comprehensive and trusted information package to help future women navigate their LS journey.
Funded in partnership with the British Society for the Study of Vulval Disease
Each year, around 7,500 women are diagnosed with Ovarian Cancer in the UK and less than 45% of these will survive beyond five years. There is an urgent need to improve survival. One of the biggest challenges is identifying who’s at highest risk of their cancer coming back after treatment, and which treatment will be most effective. Prof Ahmed Ahmed and team at the University of Oxford want to develop test that can be used with all patients to identify who’s at highest risk and suggest the best treatment for each individual person. If successful, this could improve survival rates for all women with ovarian cancer.
Endometrioid ovarian cancer (EnOC) is a rare form of ovarian cancer that affects 250 women each year in the UK. Dr Robert Hollis, based at the University of Edinburgh, is investigating the different subtypes of this cancer to find the best way of identifying which patients are at highest risk. By doing this, he hopes that it will be possible to personalise care - sparing some from side effects of treatments that don't work and designing new therapies for those who need them most.
Funded in partnership with the British Gynaecological Cancer Society

Wellbeing of Women has announced its Chair and Deputy Chair of its Research Advisory Committee.

Women make up 51% of the population, yet women’s health has not been prioritised.

Together with several funding partners, Wellbeing of Women is investing in new research studies on women’s health issues, from heavy menstrual bleeding to pregnancy care, and from the menopause to gynaecological cancers.