
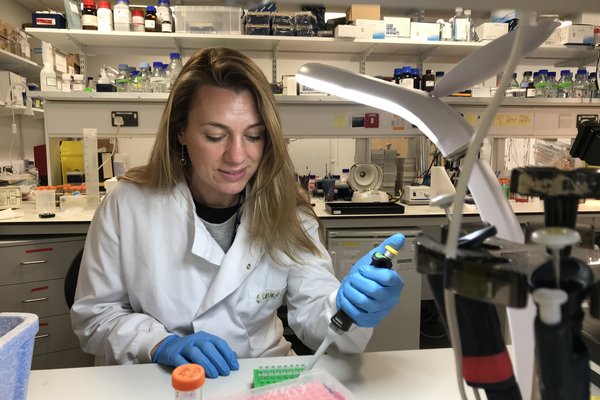
Targeting treatment resistance in ovarian cancer
Cervical cancer develops in the cervix. This is the opening of the womb (uterus) into the vagina. Cervical cancer is most common in women in their 30s, but screening can help prevent it.

Cervical cancer affects your cervix, which is part of the female reproductive system. It is sometimes called the neck or opening of the womb.
Cervical cancer happens when cells in the cervix start growing irregularly and multiply uncontrollably. The initial stages of cells changes may be called ‘abnormal cells’ and these can resolve by themselves without further action. Abnormal cells are sometimes called ‘pre-cancer’ and they can vary from what’s called minor borderline/low grade changes to high grade changes. Borderline/ low grade changes can get better on their own. Cervical cancer occurs when the cells start invading into the cervical tissues.
There are two main types of cervical cancer: squamous cell cancer and adenocarcinoma which are named after the type of cell that becomes cancerous.
Cervical cancer usually grows slowly. In people with healthy immune systems, it typically takes 15-20 years for cervical cancer to develop. Your treatment will depend on how big the tumour is and if it has spread.
There are over 3,100 cases of cervical cancer in the UK each year.
It may be helpful to familiarise yourself with the difference between the classifications of pre-cancer, the difference between pre-cancer and cancer and the different stages of cervical cancers.
Nearly all cervical cancers are caused by the human papillomavirus (HPV). HPV is the name given to a group of viruses with more than 100-different types. Not all of them are cancer causing, the ones that can cause cancer are known as high-risk HPV. HPV is very common, and most people will get the virus at some point in their life.
HPV is spread through close skin-to-skin contact during any type of sexual activity with a partner.
Most of us won’t realise we have HPV. It can stay at very low or undetectable levels for many years without causing problems. In most cases, the body’s immune system will eliminate the virus within two years. This means an HPV infection may have come from a partner a long time ago.
Cervical cancer rates in the UK are highest in women and people with a cervix aged 30–34 years. But younger and older women can still get cervical cancer so it’s important you attend screening appointments.
Although HPV is the most common risk factor for cervical cancer, there are other risk factors for developing cervical cancer:
You can reduce your risk of developing cervical cancer by attending your cervical cancer screening.
Cervical cancer often has no symptoms in its early stages. Most people are diagnosed through the NHS cervical screening programme. That’s why cervical screening is so important.
The most common symptoms of cervical cancer are:
If you have these symptoms speak to your GP, don’t wait for your next screening appointment.
Screening is one of the best ways to protect yourself from cervical cancer. Since screening started, the number of women dying from cervical cancer has halved.
Also known as a smear test, cervical screening checks the health of your cervix. It checks for high-risk HPV and if positive, the cells are looked at to see if they are pre-cancerous. It’s not a test for cancer, but it can help prevent cancer by spotting any problems early.
You’re automatically invited for screening if you are:
Trans men do not receive invitations if registered as male with their GP but are still entitled to screening if they have a cervix. Make sure you speak to your GP and ensure you are invited for screening if this applies to you.
Cervical cancer can spread to other areas of the body. That’s why it’s important to always attend your screening appointments to spot it early.
The HPV vaccine helps to protect against cancers caused by HPV and is given as one injection.
Boys and girls are offered the vaccine between 12 and 13 years old, but if they miss it for any reason, they can still get it for free on the NHS until their 25th birthday if:
The NHS website also has lots of information about the vaccine.
If your smear test found signs of abnormal cells or if you spoke to your GP about possible symptoms, you’ll have some tests.
The most common test is a colposcopy. A speculum will be placed into the vagina to enable the colposcopist to see your cervix, and a microscope with a light at the end is used to study the cervix in more detail (the microscope isn’t inserted into the vagina). The colposcopist may apply some dye to the cervix to help highlight any abnormal cells.
Depending on the result, you may have some other tests, including:
There are different treatments for cervical cancer. The best treatment will depend what type, grade and stage of cervical cancer you have.
Treatments for cervical cancer include:
If you are diagnosed with cervical cancer, it is likely that you will receive a combination of these treatments. Your doctor can discuss the options with you, and you’ll be able to ask them any questions that you might have.
It’s a good idea to discuss what your options are and the benefits and risks of each so that you can reach a decision that is best for you. Sometimes appointments can feel overwhelming, so it can be helpful to write down your questions in advance and take a second person along or ask if you can record the appointment.
For more information about cervical cancer treatments, visit the NHS website.
Cervical cancer is often treatable, but this can depend on how early the cancer is detected. As with all cancers, catching it early makes it easier to treat. That’s why it’s important to attend your screening appointments and go to your GP if you spot any symptoms.
A diagnosis of cervical cancer can be overwhelming. But there are places you can go to get support.
Jo’s Trust is a charity that has a helpline, online forum and support service.
You can also watch our webinar about preventing cervical cancer. Experts discuss what cervical cancer is and why it’s so important to attend your screening appointments.
And in our gynaecological cancers’ webinar, Dr Sarah Kitson, an expert in women’s cancers, discusses the most common symptoms of the five gynaecological cancers: cervical; ovarian; vulval; vaginal; and womb cancer. She also explains who may be most at risk and the impact a diagnosis can have.
Watch our webinar on preventing cervical cancer
Learn more about cervical cancer, from prevention to treatments in development from leading experts including Ms Theresa Freeman-Wang, a consultant gynaecologist at the Whittington Health NHS Trust, Hannah Dwyer, a Support Services Officer for Jo's Cervical Cancer Trust, and Dr Maria Paraskevaidi, Postdoctoral Research Fellow at Imperial College London.As a women’s health charity, we fund research to save and change the lives of women, girls and babies.
Our research played a part in establishing the link between HPV and cervical cancer, resulting in the first preventative school-wide vaccination programme.
And we are currently co-funding a research study with the British Gynaecological Cancer Society to investigate if an innovative new technology can help detect and treat cervical and vulval cancers faster and more accurately.






The vulva is the external part of the female genitals. Cancer in this area can cause a lump that may be sore or bleeding. There are 1,400 new cases in the UK every year.

Ovarian cancer is cancer of the ovaries or fallopian tubes. Symptoms include tummy pain, bloating, reduced appetite and needing to pee more often.

Most womb cancer starts in the lining of the uterus (womb). Around 9,700 women are diagnosed with womb cancer each year in the UK. The most common symptom is unusual bleeding from the vagina.