
Wellbeing of Women announces Professor Hilary Critchley as the new Research Advisory Committee Chair
Wellbeing of Women has announced its Chair and Deputy Chair of its Research Advisory Committee.
Wellbeing of Women funded Dr Cornish's early research on a rare placental disorder

We are very pleased to announce that Dr Emily Cornish has won the MRC Max Perutz Science Writing Award 2022 for her essay on a rare placental disorder called chronic histiocytic intervillositis (CHI) which can lead to recurrent pregnancy loss.
Dr Cornish's early stage research into CHI was funded by Wellbeing of Women. Her award winning essay can be read below.
By Dr Emily Cornish
Amy’s third baby was born in the middle of the night. In the split second before he cried, everyone in the operating theatre held their breath. I was lurking in a corner holding a huge bucket of ice, waiting to collect the placenta. The stakes felt incredibly high. Baby William’s two sisters were stillborn because of a placental disorder called chronic histiocytic intervillositis (CHI).
Most obstetricians have never heard of CHI. It’s a rare condition that affects one in 2,000 pregnancies and can only be diagnosed postpartum by examining the placenta under a microscope. The aim of my PhD is to discover the cause of this disease.
In a healthy pregnancy, the mother’s blood flows through the placenta in a channel called the intervillous space, where it comes into direct contact with tree-like branching structures known as placental villi. This is where the vital exchange of gases and nutrients between the mother and baby occurs. In CHI, the channel gets clogged with maternal immune cells, impairing the exchange process and leading to serious consequences for the baby. Only half of these pregnancies result in a live birth and some babies have to be delivered several months early by emergency caesarean to give them a chance of survival.
CHI is a rare condition that affects one in 2,000 pregnanciesCHI usually affects women who are fit and well, with no medical problems. It comes out of the blue and has a devastating impact on couples hoping to have a baby. The cruellest thing about CHI is that eight times out of 10, it will recur in a subsequent pregnancy.
Any miscarriage or stillbirth is emotionally shattering for the parents, but for most it is unlikely to happen again. This is where CHI is different. When Amy received the diagnosis after her second daughter was stillborn, she experienced a “double grief”: not just for the loss of Grace, but for the loss of the future and the family she had envisaged. There are no tests that can reliably predict the recurrence of CHI, so these subsequent pregnancies require incredibly close monitoring. Many women will have scans every fortnight, battling to suppress their dread as they return to the same ultrasound departments where their previous losses were diagnosed.
The cause of CHI is unknown. However, when you look at a placenta with CHI through a microscope, at a cellular level, it looks remarkably similar to a rejected kidney transplant. My hypothesis is that affected mothers make an antibody that attacks the developing placenta. This leads to inflammation of the placenta and an influx of maternal immune cells. Support for this theory comes from the fact that when couples affected by CHI undergo IVF using their own eggs and sperm, and transfer the embryo into a surrogate, the pregnancy progresses normally with no signs of CHI. This confirms that the problem derives from the mother’s immune system.
Initially, designing a research study focusing on CHI felt daunting – how could I expect to recruit meaningful numbers of women when the disease is so rare? Luckily, I was rescued by a woman named Claudia and a Facebook group.
Claudia lost four sons to CHI in the space of three years. As she navigated through the heartache of learning to live without her children, she became determined to raise the profile of this mysterious and brutal disease. Since then, she has been a tireless advocate for advancing research into CHI and helps to run a Facebook support group for affected women. The group has more than 700 members and is a lifeline for parents struggling to come to terms with their diagnosis.
Despite its rarity, and thanks to Claudia’s group, I have managed to recruit more than 30 women to my study. I collect blood and placental samples from them to look for unusual immune cells, proteins or antibodies that could explain what goes wrong in their pregnancies. I also analyse their DNA to look for variations in their genetic code that might predispose them to CHI.
Any miscarriage or stillbirth is emotionally shattering for the parents, but for most it is unlikely to happen again. This is where CHI is differentBy purifying antibodies from their blood and comparing them with women who have had healthy, uncomplicated pregnancies, I have shown that women with CHI react abnormally to placental proteins. My next challenge is to determine exactly what triggers this reaction and unravel the molecular basis of how this leads to catastrophic placental damage. And the ultimate goal is to use this knowledge to develop new, targeted treatments that can prevent recurrence.
My team is already making progress on the final question. Claudia lost her children 10 years ago and eventually resorted to surrogacy, as nothing her doctors tried could stop the relentless recurrence of CHI. However, over the last few months we have become cautiously optimistic about a new treatment protocol that involves suppressing the mother’s immune system during pregnancy. Once again, we drew on the parallels between CHI placentas and rejected transplants. This treatment is the same one that people with organ transplants take to stop their bodies rejecting the donated organ. It’s an intensive cocktail of medication that requires regular blood tests and close vigilance for early signs of potentially dangerous side-effects. We have only treated a handful of women so far, but the majority have gone home with a healthy baby.
But until we discover the cause of CHI, these treatments are, at best, an educated guess. I’m only nine months into my PhD and am well aware that finding a miracle cure is an unrealistic dream. However, my vision is to make concrete advances in our understanding of CHI so that future treatments can be tailored towards the precise defect in affected women’s immune systems.
Until we discover the cause of CHI, treatments are, at best, an educated guessAfter Amy lost her daughters, she felt like she’d been “kicked out of the motherhood club”. She couldn’t bear to lose another baby and although the prospect of a heavily medicated pregnancy filled her with anxiety, she decided to take the gamble. Amy took more than 1,000 tablets and injected herself with a blood thinner at least 200 times during her pregnancy with William. She travelled to the hospital on commuter trains during the pandemic, came to scans alone because of the restrictive Covid visiting policy and had blood tests almost every week.
I am inspired and humbled by the extraordinary courage and determination of the women who embark on this regime. CHI has been neglected by obstetric researchers, but thankfully the women who have experienced it are highly motivated and desperate to educate us. If my research can draw attention to the massive impact of CHI and give affected families some hope, then spending my evenings crouching in an operating theatre with an ice bucket seems entirely worthwhile.
Read about the MRC Max Perutz Science Writing Award 2022
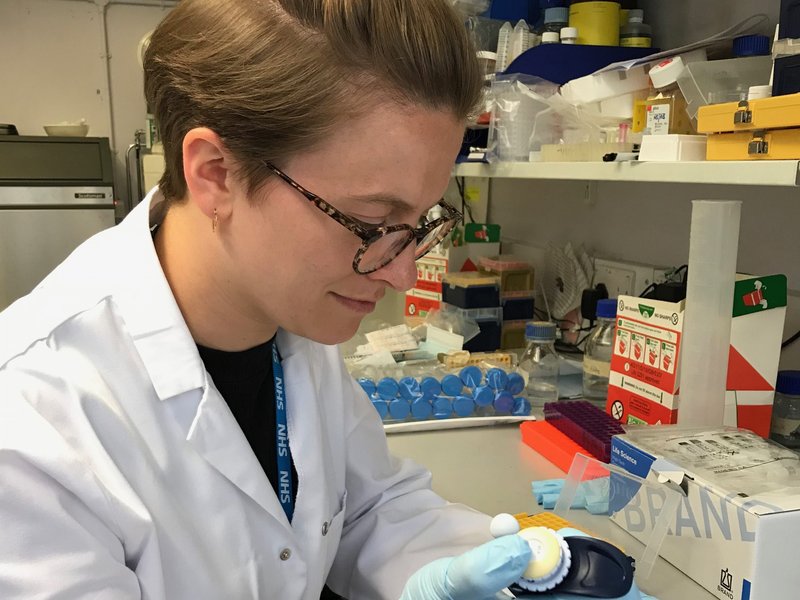
Main image: Dr Emily Cornish with Ian Tucker, Science and Tech Editor of the Observer. Credit: Joel Knight

Wellbeing of Women has announced its Chair and Deputy Chair of its Research Advisory Committee.

We’re delighted to announce the funding of 17 new research projects tackling health inequalities and spanning the whole life course – from menstruation to menopause, pre-natal to postnatal, and gynaecological cancers.

Women make up 51% of the population, yet women’s health has not been prioritised.